Ever get “butterflies” in your stomach when you’re nervous?
Or feel nauseous after a stressful day?
These experiences highlight the powerful connection between our gut and brain.
With functional medicine: abdominal and mental health are intimately connected…
…revolutionizing holistic well-being.
Let’s look into the connection between gut & mental health.
And how functional medicine tackles it.
How Are Gut Health and Mental Health Connected?
The connection between gut health and mental health is facilitated by the gut-brain axis, a sophisticated communication network that links the viscera and brain.
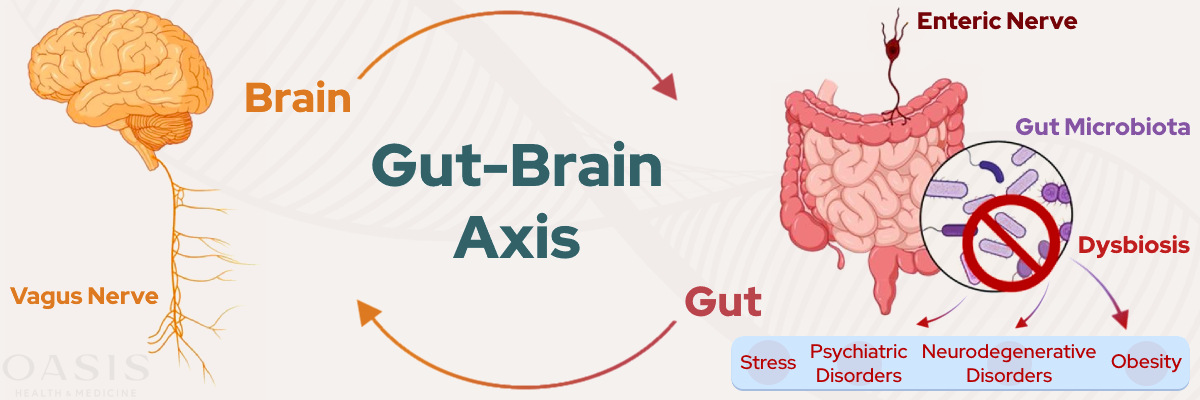
This pathway runs primarily through Cranial Nerve 10, aka the vagus nerve.
What’s it do?
This intricate bidirectional pathway allows signals to travel in both directions, impacting both digestive health and mental well-being.
What’s the gut’s role?
The gut is responsible for producing neurotransmitters such as serotonin and dopamine.
They play a crucial role in regulating mood.
- Serotonin: A chemical messenger that helps regulate mood, emotions, appetite, sleep, pain perception, and social behavior.
- Dopamine: A neurotransmitter involved in pleasure, reward, motivation, movement control, learning, and memory consolidation.
Therefore: maintaining a healthy gut can significantly contribute to a happier and more balanced mind.

There’s more than just serotonin and dopamine:
Emerging research continues to explore the depth of this connection.
This highlights the importance of gut health in overall mental health maintenance.
Understanding this relationship is vital for developing holistic approaches…
…to mental well-being that consider the profound impact of dietary choices and gut health on emotional states.

Why Are Gut Issues So Prevalent?
The prevalence of gut issues in today’s society can be attributed to various modern lifestyle factors.
Diets rich in:
- Processed foods
- High in sugars
- Unhealthy fats
- Along with increased stress levels
- Overuse of antibiotics
…have significantly disrupted the natural balance of good and bad bacteria within our gut microbiome.
These disruptions can lead to a host of issues.
Such as intestinal permeability aka “leaky gut”.
Leaky gut is where the gut lining becomes permeable, allowing toxins and undigested food particles to enter the bloodstream.
In short:
Candida overgrowth and other imbalances can compromise immune function and nutrient absorption – a lack of fiber and prebiotics, essential for gut health – further exacerbates these problems.
Bottom line:
Addressing these concerns requires a multifaceted approach that promotes a balanced diet, stress management, and mindful antibiotic use to restore and maintain a healthy gut environment.
Why Are Mental Health Issues So Prevalent?
The rising prevalence of mental health issues can be attributed to a complex interplay of factors.
These include the stresses of modern life, dietary inadequacies, and sedentary lifestyles. Increased stress from:
- Work
- Social pressures
- Economic instability
Can contribute to conditions such as:
- Anxiety
- Depression
- Chronic stress.

Furthermore, poor dietary habits that lack essential nutrients, coupled with insufficient physical activity, can negatively impact brain health and emotional resilience.
Then again, the fast-paced nature of contemporary life often leaves little room for reflection or self-care, compounding mental health struggles.
Addressing these challenges involves fostering environments that prioritize mental well-being through:
- Balanced nutrition
- Regular exercise
- Supportive communities
- Accessible mental health services.
Why Do Gut Health and Mental Health Issues Go Together?
Gut health and mental health are intricately linked.
Together, they often create a feedback loop.
This feedback loop can either be detrimental or beneficial depending on the state of each.
As an example, take poor gut health…
It’s characterized by an imbalance in gut flora or an unhealthy gut lining, can lead to mental health challenges by affecting the production and regulation of mood-related neurotransmitters.
Consider this:
Mental health issues such as stress, anxiety and ADHD can negatively impact gut health.
Which leads to: digestive issues and further exacerbating mental health conditions.
This cycle highlights the importance of addressing both gut and mental health simultaneously.
But that’s not all:
When efforts are made to improve one, it often positively influences the other, creating a virtuous cycle of enhanced overall health and well-being.
Interventions that support gut health through:
|
|
Can lead to significant improvements in quality of life.

Gut Testing Is Done Through A Comprehensive Stool Analysis
Here’s a list of some of the markers that are tested:
- Zonulin: is a protein that plays a crucial role in regulating gut permeability.
- Calprotectin: is a protein found in white blood cells and is a reliable marker for inflammation in the intestines.
- Candida: is a type of yeast that naturally resides in the gut.
- Parasites and H. Pylori: are organisms that can cause significant disturbances in the gut.
- Commensal and Opportunistic Bacteria: are beneficial bacteria that aid in digestion, nutrient absorption, and immune function – while harmful bacteria can cause infections and inflammation.
- Anti-Gliadin IgA: are antibodies that indicate sensitivity to gluten, a protein found in wheat and other grains.
- Secretory IgA: acts as the first line of defense against pathogens by preventing their adherence to the intestinal lining.
- Pathogenic Bacteria: are harmful bacteria that can disrupt the natural balance of the gut microbiota, leading to symptoms like diarrhea, abdominal pain, and fever.
Food Sensitivity Testing (IgG Blood Testing)
Food sensitivities are a common issue that many individuals experience, yet they often go unnoticed or misdiagnosed.
Despite being overlooked, these sensitivities can have a profound impact on both gut health and mental health conditions.
Let’s look at it in detail:
Consuming foods that your body is sensitive to can lead to digestive discomfort, such as bloating, gas, or diarrhea.

Well… this can also exacerbate mental health issues like anxiety and depression.
IgG blood testing: is one effective way to identify these food sensitivities.
(This type of test can detect specific antibodies in your blood that are produced in response to certain foods.)
Here’s the thing.
By pinpointing which foods trigger these responses…
…individuals can gain valuable insights into what might be causing their symptoms.
Pro Tip: People can take proactive steps to eliminate or reduce the intake of these problematic foods, which leads to – improved health outcomes and a general sense of feeling better. |
So, understanding and managing food sensitivities can be transformative.
Or put another way:
When individuals identify their specific triggers…
…they can make informed dietary changes that alleviate symptoms and enhance their quality of life.

What this means is:
Someone suffering from chronic fatigue or digestive issues might find relief simply by adjusting their diet.
Moreover, these adjustments can lead to:
- Increased energy levels
- Better mood
- More balanced mental state.
Now, for those interested in the topic of testing oneself for food sensitivities, explore our post on food sensitivity testing.
SIBO Breath Testing – The Surprising Link Between Gut Health and Mental Wellbeing
Did you know?
Small Intestinal Bacterial Overgrowth (SIBO) is a condition that significantly impacts both gut and mental health.
This condition arises when bacteria translocate from the large intestine into the small intestine.
This leads to: Excessive bacterial growth in an area typically not meant for such a dense population.
Important Note: The imbalance can lead to a wide array of symptoms, most commonly including bloating and abdominal pain.
These symptoms occur because the excessive bacteria ferment ingested food:
- Creating gasses like hydrogen and methane.
- Which lead to discomfort and distention in the abdomen.
Beyond physical symptoms, SIBO also affects mental health.
Mood Disturbances, Anxiety & Depression Via The Gut
An imbalance in gut bacteria, such as that caused by SIBO, can result in mood disturbances, anxiety, and depression.
This is due to:
The bacteria’s influence on nutrient absorption, neurotransmitter production, systemic inflammation, and the integrity of the gut barrier.

SIBO Breath Test
It’s one of the primary methods for diagnosing SIBO.
This non-invasive procedure involves the patient ingesting a substrate like glucose or lactulose and then measuring the levels of hydrogen and methane in their breath over a few hours.
So You Know: These gasses are byproducts of bacterial fermentation and their presence in higher-than-normal amounts indicates bacterial overgrowth in the small intestine.
In fact:
The test is crucial as it helps in accurately diagnosing the condition.
Because, SIBO is often misattributed to other gastrointestinal disorders.
The big takeaway?
Once SIBO is identified, it allows for the development of targeted treatment plans tailored to the individual’s specific bacterial profile.

Plus, treatment often include:
- Antibiotics
- Herbal antimicrobials
…to reduce bacterial numbers – as well as dietary changes to support gut health.
The FODMAP Diet: Helps to decrease the intake of fermentable carbohydrates that feed the bacteria. They include short chain carbohydrates and sugar alcohols that are poorly absorbed by the body, that can result in abdominal pain and bloating. |
Bottom Line?
Restoring gut balance can alleviate both the gastrointestinal symptoms and the related mental health effects.
Leading to: an overall improvement in quality of life.
Undertaking a SIBO treatment is crucial for individuals who suffer from persistent gastrointestinal issues, often accompanied by mental health challenges.
Functional Medicine VS. Conventional Medicine
Let’s start with conventional medicine.

Conventional Medicine
It’s a well-established and widely practiced approach that…
…primarily focuses on diagnosing and treating symptoms of various ailments and diseases.
It often relies on:
- medications
- surgeries
- other interventions
to manage and alleviate symptoms – thereby providing relief and improving patients’ quality of life.
However, this approach may not always get to the heart of the problem.
This Approach: Often addresses the symptoms rather than the underlying causes of health issues.
In addition, conventional medicine can sometimes become “siloed,” focusing narrowly on specific symptoms without considering the broader context of a patient’s health.
Functional Medicine
Functional medicine, on the other hand, offers an alternative approach.

It aims to: identify and treat the root causes of health concerns.
This holistic method goes beyond symptom management.
Functional medicine aims to understand the complex interactions within the body’s systems…
…considering factors such as genetics, environment, and lifestyle.
How so?
Simply by, evaluating these interconnections.

Functional medicine for gut health and better mental health starts from within, where the gut microbiome plays a crucial role in regulating mood, emotions, and cognitive function for achieving optimal mental health.
Functional medicine practitioners develop personalized treatment plans that focus on the individual as a whole, rather than just isolated symptoms.
Comprehensive Holistic Care: The Power Of Combining Traditional And Functional Medicine
At Oasis Health and Medicine, we embrace the principles of functional medicine.
Our doctors recognize and respect the significant contributions of conventional medicine.
It’s important to note:
In acute care settings – conventional medicine plays an indispensable role.
(This is where immediate intervention is crucial.)

Think about it like this:
We believe that integrating both approaches can provide the best possible outcomes for our patients.
As they complement each other in addressing both immediate and long-term health needs.
Gut Balance With Functional Medicine: The Key to Optimal Health
Understanding the intricate gut-brain connection through the lens of functional medicine offers a revolutionary and comprehensive approach to achieving optimal health.
Imagine a pathway:
Where your physical and mental well-being are not treated in isolation.
But rather – as interconnected elements of your overall health journey.
This approach allows us to dive deeper into how our digestive and neurological systems interact.
Impacting everything from mood to immunity.

If you’re ready to take charge of your health and explore the profound benefits of functional medicine…
…we invite you to book a discovery call with one of our expert Naturopathic Doctors.
Schedule Your Discovery Call ➜
Our team is dedicated to guiding you through a personalized health plan.
Which addresses:
Not just symptoms, but the root causes of health issues.
References:
https://www.sciencedirect.com/science/article/pii/S1756464623005157/
https://pubmed.ncbi.nlm.nih.gov/36232548/
https://pubmed.ncbi.nlm.nih.gov/34450312/
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC10084985/
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC9709456/